Introduction to Pancreatitis
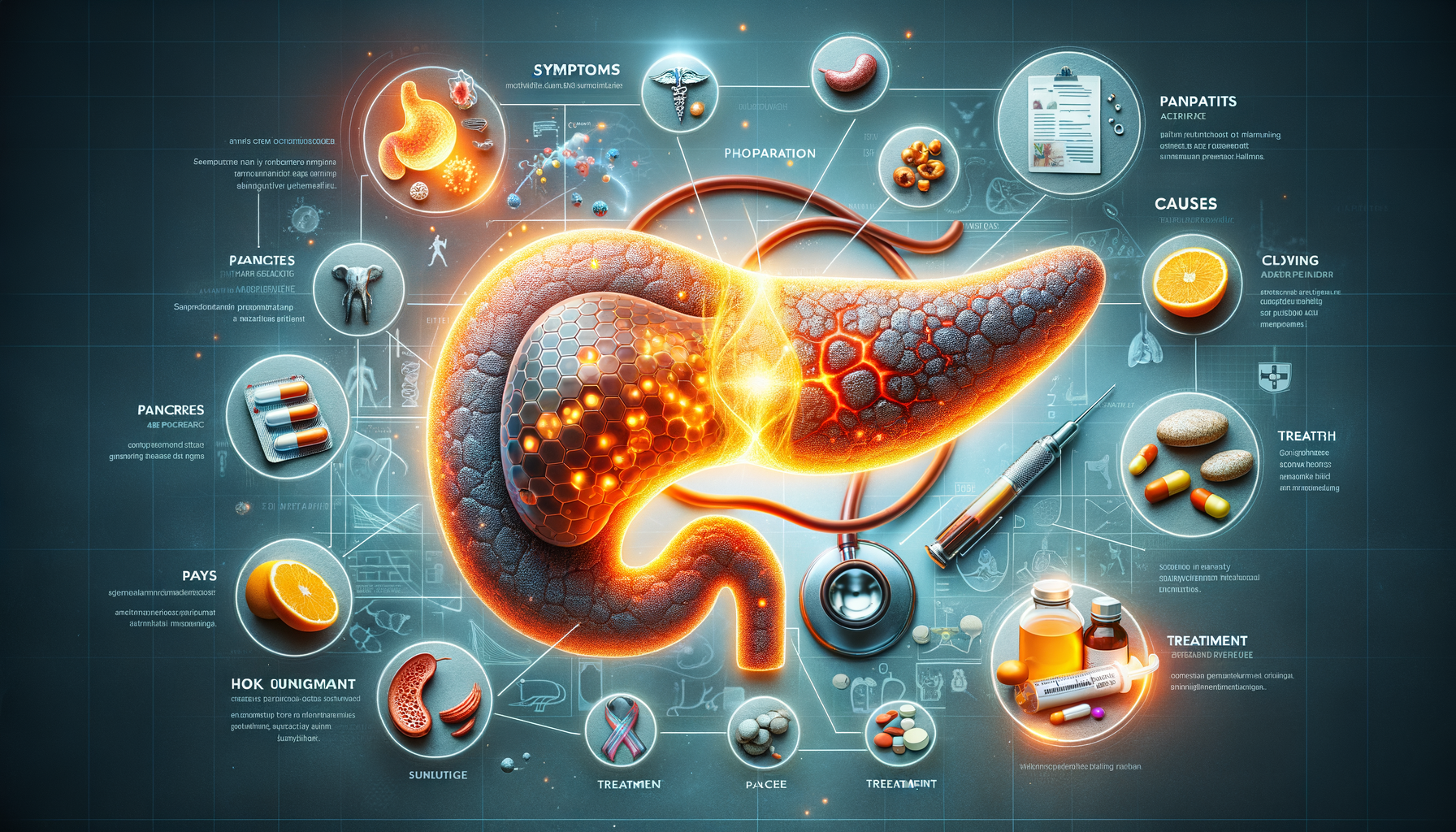
Pancreatitis is a medical condition characterized by the inflammation of the pancreas, an essential organ that plays a critical role in digestion and blood sugar regulation. This condition can manifest as acute or chronic, each with its own set of complications and treatment protocols. Understanding pancreatitis is crucial because it affects not only the digestive system but also overall health, potentially leading to severe complications if not managed properly.
The pancreas, located behind the stomach, produces enzymes that aid in digestion and hormones such as insulin, which regulate blood sugar levels. When the pancreas becomes inflamed, these enzymes can start digesting the pancreas itself, leading to pain and swelling. The inflammation can be triggered by various factors, including gallstones, alcohol consumption, and certain medications. Recognizing the symptoms and seeking timely medical intervention is vital to prevent further complications.
Symptoms of Pancreatitis
The symptoms of pancreatitis can vary depending on whether the condition is acute or chronic. Acute pancreatitis often presents suddenly and may include:
- Severe abdominal pain that may radiate to the back
- Nausea and vomiting
- Fever
- Increased heart rate
- Swollen and tender abdomen
Chronic pancreatitis, on the other hand, develops over time and may lead to persistent symptoms such as:
- Chronic abdominal pain
- Unintended weight loss
- Oily, foul-smelling stools (steatorrhea)
- Diabetes
These symptoms can significantly impact a person’s quality of life, making early diagnosis and management crucial. If you experience any of these symptoms, it is important to consult a healthcare professional for a thorough evaluation and appropriate treatment plan.
Causes and Risk Factors
Understanding the causes and risk factors of pancreatitis is essential for prevention and management. The most common causes include:
- Gallstones: These can block the pancreatic duct, leading to inflammation.
- Alcohol consumption: Excessive alcohol intake is a major risk factor, particularly for chronic pancreatitis.
- Certain medications: Some drugs can induce pancreatitis as a side effect.
- Genetic factors: Some individuals may have a genetic predisposition to pancreatitis.
- High triglyceride levels: Elevated levels can increase the risk of developing pancreatitis.
Apart from these, other factors such as smoking, obesity, and certain medical conditions like cystic fibrosis can also contribute to the development of pancreatitis. Identifying and modifying these risk factors can help in reducing the likelihood of pancreatitis episodes.
Treatment Options for Pancreatitis
Treating pancreatitis involves managing symptoms, addressing the underlying cause, and preventing complications. The treatment approach may vary based on the severity and type of pancreatitis.
For acute pancreatitis, initial treatment usually involves:
- Hospitalization for monitoring and supportive care
- Fasting to rest the pancreas
- Intravenous fluids to prevent dehydration
- Pain management
Once the acute phase is managed, addressing the underlying cause, such as removing gallstones or managing alcohol intake, is crucial to prevent recurrence.
Chronic pancreatitis treatment focuses on managing pain and nutritional deficiencies. This may include:
- Pancreatic enzyme supplements to aid digestion
- Dietary modifications to ensure adequate nutrition
- Pain management strategies
- Addressing complications such as diabetes
In some cases, surgical interventions may be necessary to relieve obstructions or remove damaged tissue. A multidisciplinary approach involving gastroenterologists, dietitians, and pain specialists can provide comprehensive care for individuals with pancreatitis.
Living with Pancreatitis: Lifestyle and Management
Managing pancreatitis requires a commitment to lifestyle changes that support pancreatic health and prevent flare-ups. Here are some strategies:
- Adopt a balanced diet: Focus on low-fat meals that are rich in fruits, vegetables, and whole grains.
- Limit alcohol intake: Avoiding alcohol is crucial, especially for those with a history of alcohol-induced pancreatitis.
- Quit smoking: Smoking can exacerbate pancreatitis and increase the risk of complications.
- Stay hydrated: Adequate fluid intake supports overall health and digestion.
- Exercise regularly: Moderate physical activity can help maintain a healthy weight and reduce stress.
Regular follow-ups with healthcare providers are essential to monitor the condition and adjust treatment plans as needed. By adopting these lifestyle changes, individuals with pancreatitis can improve their quality of life and reduce the risk of complications.